Type 1 diabetes occurs when the pancreas does not make enough or any insulin. Type 2 diabetes occurs when the body cannot use insulin properly.
In this article, we look at how the pancreas is involved in diabetes. We also describe the complications of diabetes related to pancreatic and other organ disorders.
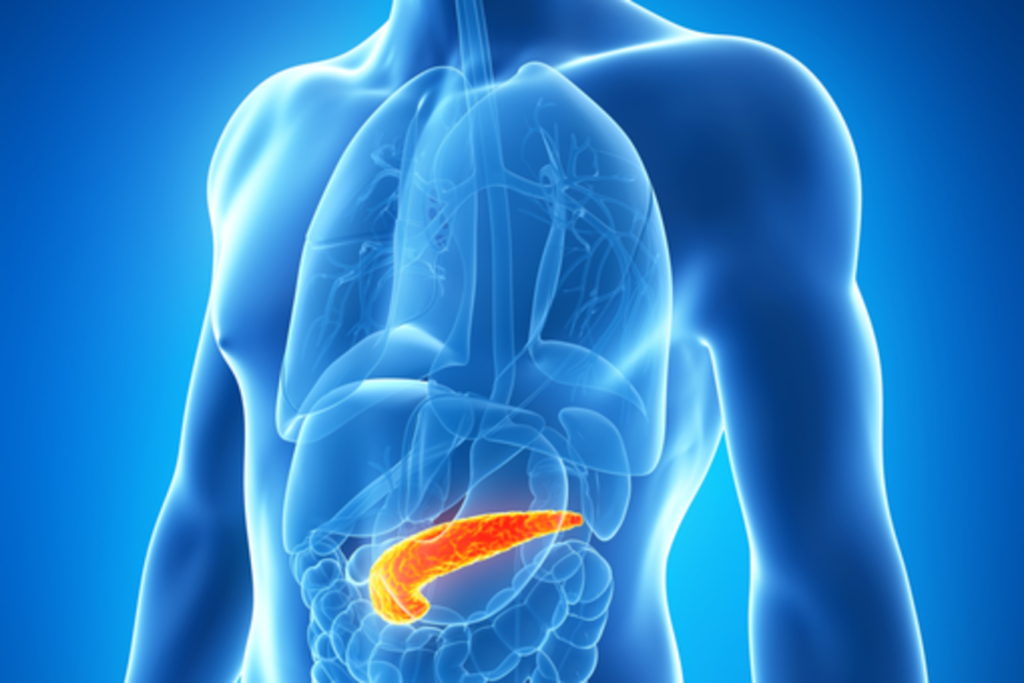
What to Know About the Pancreas
The pancreas produces digestive enzymes, and is located in the abdomen, behind the stomach.
It also produces insulin, a hormone that helps regulate blood sugar levels. The cells that produce insulin are called beta cells. They are located in the islets of Langerhans, a collection of structures within the pancreas.
Insulin helps the body use the carbohydrates in food for energy. It transports glucose from the blood to the cells of the body. Glucose gives cells the energy they need to function.
If the body has too little insulin, the cells cannot take up glucose from the blood. As a result, the level of glucose in the blood increases. A doctor may refer to this as high blood sugar or hyperglycemia.
Hyperglycemia is responsible for most of the symptoms and complications of diabetes.
How is the Pancreas Linked With Diabetes?
Diabetes is characterized by high blood sugar. It results from insufficient insulin production or function, which can be a side effect of pancreatic problems.
People with diabetes have high or low blood sugar levels at different times, depending on what they eat, how much they exercise, and whether they take insulin or diabetes medication.
Both type 1 and type 2 diabetes involve the pancreas.
Type 1 Diabetes
Type 1 diabetes occurs when the pancreas does not make enough, or any, insulin. Without insulin, cells cannot get enough energy from food.
This form of diabetes results from the body’s immune system attacking the insulin-producing beta cells in the pancreas. Beta cells become damaged and over time the pancreas stops producing enough insulin to meet the body’s needs.
People with type 1 diabetes can balance their blood glucose levels with daily insulin injections or an insulin pump.
Doctors once called this type “juvenile diabetes” because it often develops in childhood or the teenage years.
There is no clear cause of type 1 diabetes. Some evidence suggests that it is caused by genetic or environmental factors. An estimated 1.25 million people in the United States are living with type 1 diabetes.
Type 2 Diabetes
This type occurs when the body develops resistance to insulin. Although the pancreas can still produce the hormone, the body’s cells cannot use it effectively.
As a result, the pancreas produces more insulin to meet the body’s needs, and it often fails to meet the increased demand.
With an insufficient amount of insulin in the body, diabetes develops. Over time, beta cells become damaged and may stop producing insulin altogether.
Like type 1 diabetes, type 2 can cause high blood sugar levels and prevent cells from getting enough energy.
Type 2 diabetes can result from genetics and family history. Lifestyle factors, such as obesity, lack of exercise and poor diet, also play a role. Treatment often involves increasing exercise levels, improving diet, and taking certain prescription medications.
A doctor may be able to detect type 2 diabetes early, in a stage called prediabetes. A person with prediabetes may be able to prevent or delay the onset of the condition by making changes to their diet and exercise routine.
Gestational Diabetes
Pregnancy can cause type 2 diabetes, known as gestational diabetes. This can result in complications during pregnancy and delivery.
After birth, gestational diabetes usually goes away, although it increases the risk of developing type 2 diabetes later in life.
Diabetes and Pancreatitis
Pancreatitis causes inflammation of the pancreas and is of two types:
- Acute pancreatitis, in which symptoms appear suddenly and last for a few days.
- Chronic pancreatitis, a long-term condition in which symptoms come and go for many years.
Chronic pancreatitis can damage the cells of the pancreas and lead to diabetes.
Pancreatitis is treatable, but severe cases may require hospitalization. A person should take pancreatitis seriously, as it can be life-threatening.
Symptoms of pancreatitis include:
- vomiting
- abdominal tenderness
- pain that feels worse after eating
- nausea
- fever
- pain in the upper abdomen that can radiate toward the back
- a racing pulse
Diabetes And Pancreatic Cancer
According to the Pancreatic Cancer Action Network, people who live with diabetes for 5 or more years are 1.5 to two times more likely to develop pancreatic cancer.
Onset of type 2 diabetes later in life can be a symptom of this type of cancer. Another symptom includes having trouble controlling blood sugar levels after they are well controlled.
The relationship between diabetes and pancreatic cancer is complex. Diabetes increases the risk of developing this type of cancer, and pancreatic cancer can sometimes lead to diabetes.
Other risk factors for pancreatic cancer include:
- obesity
- a poor diet
- aging
- genetics
- smoking
In its early stages, this type of cancer can cause no symptoms. Doctors often diagnose it when it is more advanced.
Other Disorders of the Pancreas
Cystic fibrosis can lead to the development of insulin-dependent diabetes.
In a person with cystic fibrosis, the sticky mucus causes scar tissue to form on the pancreas, and the scarring can prevent the organ from producing enough insulin. As a result, a person can develop cystic fibrosis-related diabetes (CFRD).
Signs and symptoms of CFRD are similar to those of cystic fibrosis. A person may not know they have CFRD until they undergo a routine test for diabetes.
Summary
Diabetes is related to the pancreas and insulin. Too little insulin can cause high blood sugar, which is responsible for the symptoms of diabetes.
Over time, repeated episodes of high blood sugar can lead to serious complications, which is why people with diabetes should monitor their blood sugar levels.
Certain chronic conditions, such as pancreatitis and cystic fibrosis, can cause type 2 diabetes.
A person can avoid type 2 diabetes by not smoking, maintaining a healthy weight, eating a healthy diet and exercising regularly.
Both type 1 and type 2 diabetes are manageable. Lifestyle changes and medications can help people manage their symptoms.










1 comment